We publish the proceedings report of “The Double Burden of Diseases and Challenges on Service Provision and Integration in Ethiopia: Evidence Generated from Different Experiences” workshop organized by the Ethiopian Ministry of Health and AICS Addis Ababa on 26 and 27 February 2020.
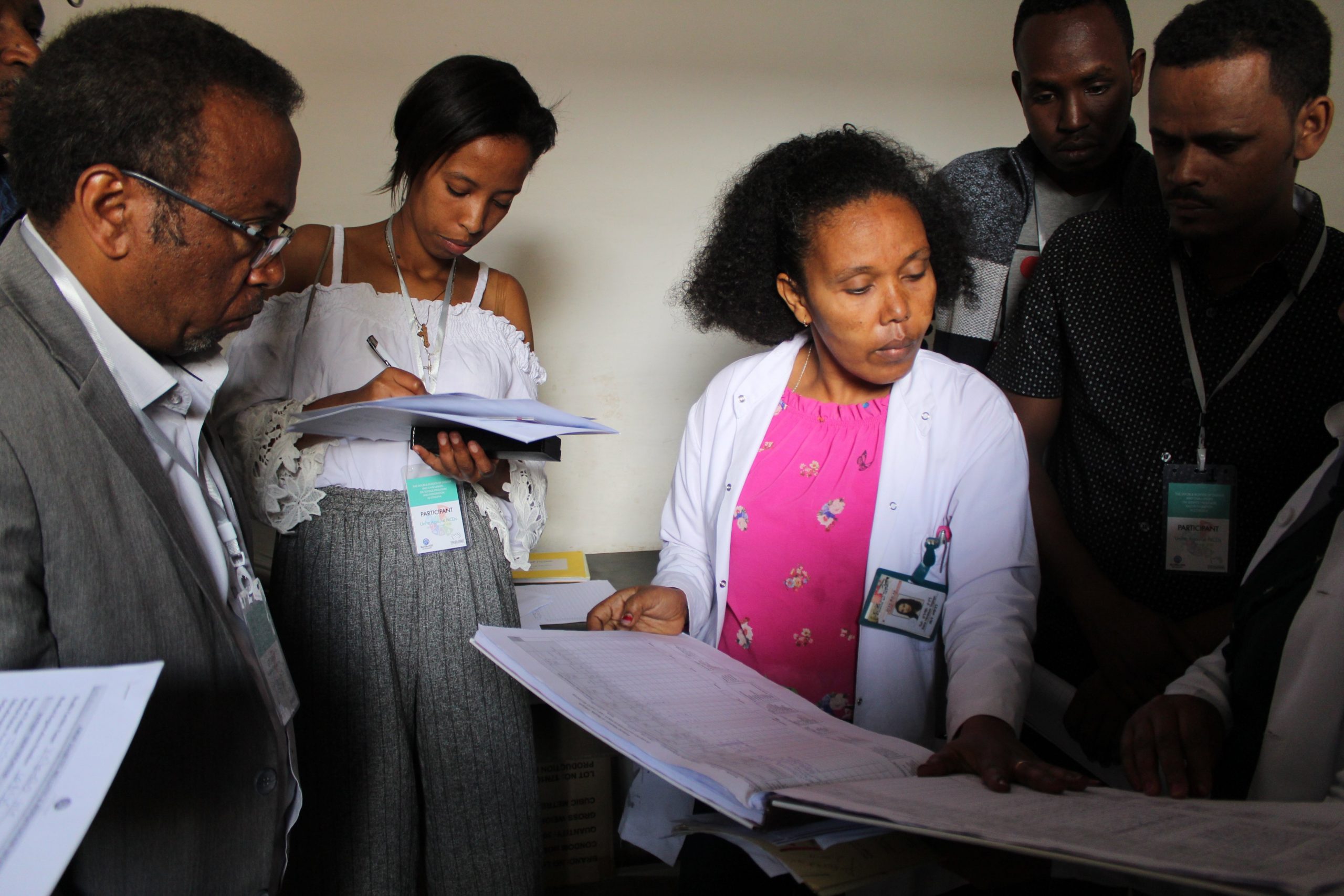
The two-day workshop saw the participation of 56 attendants and 17 experts from Government institutions, UN Agencies, Civil Society Organizations (CSOs), Universities and Health Institutions, including two international guests respectively from Sudan, Dr. Osama Head of Family Medicine Program, FMoH of Sudan, and from Palestine, Cristina Natoli the Head of AICS Jerusalem.
The former Ethiopian State Minister - now Minister - of Health Dr. Lia Tadesse together with the former Head of AICS Addis Abeba, Mr. Tiberio Chiari, opened the works reminding the importance of the event within the wider national context and the continuous support by the Italian cooperation in the health sector in the last 15 years.
12 are the key recommendations from presentations, questions, panel discussions, and sharing among experts and participants, in order to inform policymakers and strengthen the fight against Non-Communicable Diseases (NCDs) in Ethiopia:
- The rise of Non-Communicable Diseases in Ethiopia requires a multi-sectoral response for their prevention and control. There is a need for higher engagement of different sectors and stakeholders through the establishment of effective and efficient structures at national and regional levels (ex. inter-ministerial and/or parliamentary committees). Moreover, barriers to multi-sectoral actions such as lack of awareness in different sectors, low political commitment, poor coordination among stakeholders, and inadequate resources should be tackled.
- Governments should integrate NCDs as part of primary health care. The Government can facilitate managing NCDs at an early stage and, therefore, it is a less expensive investment than diagnosing and managing them at a later stage. Investments in NCDs prevention and control should also be done through evidence-based approaches so as to contribute to the strengthening of the health system in the long run.
- NCDs remain one of the most underfunded programs. Nevertheless, considering the depth and magnitude of the problem and considering that it is currently on the rise, adequate resources should be mobilized to increase budgetary allocations for addressing these diseases.
- CSOs have long contributed towards reaching public health goals and they continue to have an important role in service delivery, awareness creation, advocacy, monitoring, and accountability. There is, therefore, a need to strengthen CSOs engagement and actions in the prevention and control of NCDs. Furthermore, their expertise should be leveraged also through partnerships with the Government. Strengthen the action and contribution of NCD civil society CSOs, which should be leveraged by the engagement of governments and partnership with CSOs.
- Create partnership and collaboration with Overseas Development Assistance (ODAs) to complement domestic resources to increase health expenditure in tackling the double burden of diseases consistent with the Country’s priorities.
- Increase commitment for integration and decentralization of NCD services in the Primary Health Care (PHC) System.
- Develop appropriate strategic health communications campaigns on NCD and conduct concrete and continuous awareness creation and massive community mobilization.
- Malnutrition and unhealthy diets are one of the leading risk factors for non-communicable diseases. It is recommended to design and implement double and triple duty action interventions and programs that can simultaneously address the risk or burden of both undernutrition and overweight, obesity, or diet-related NCDs.
- Strengthen the capacity of NCD human resources through the introduction of Family Medicine curricula. Moreover, it is important to implement different retention mechanisms of trained staff.
- Ensure a continuum of delivery of drugs and supplies for NCDs, including maintenance of equipment.
- Look for innovative approaches that contextualize NCDs service delivery and identify the risk factors to design appropriate interventions.
- Strengthen the capacity of the PHC system in providing the continuity of care needed by patients affected by chronic diseases.
To read the full proceedings report, download it here.
--
Press review:
Live tweet of the workshop here
EBC TV interview to Dr. Lia Tadesse and Tiberio Chiari here (from min. 34:30)
The article on ENA here